Blog
My step by step approach to overcoming acute and chronic pain
The more I know about pain, the less afraid I am of it, so the less I notice it. This is just one person’s story, but there are many MANY people who have chronicled almost exactly the same outcome from many different causes in book form. Google “overcoming chronic pain” and tens of books spring up, almost all telling the same process.
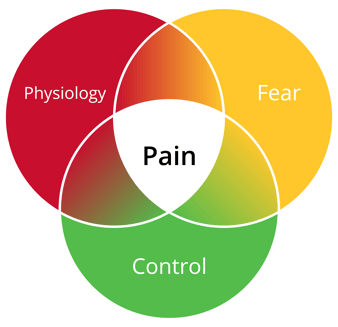 My pain came from injuries, and was easier to cope with because I caused it. Particularly after fracturing my neck (twice) and ripping a few rotator cuff muscles, pain does come visit me again from time to time, but now that I have a plan and practice it’s never as bad. Unquestionably, the more I learned about connectomes preparing for my TED talk, the better I was able to handle pain. If you haven’t seen the talk, go see it now to make the rest of the blog make more sense. The concept is that there are ways to reduce the nerve messages to the brain (physiology), but the fear and control memories connected to previously experiences are most of what you feel. Control what you expect to experience, and pain is reduced.
My pain came from injuries, and was easier to cope with because I caused it. Particularly after fracturing my neck (twice) and ripping a few rotator cuff muscles, pain does come visit me again from time to time, but now that I have a plan and practice it’s never as bad. Unquestionably, the more I learned about connectomes preparing for my TED talk, the better I was able to handle pain. If you haven’t seen the talk, go see it now to make the rest of the blog make more sense. The concept is that there are ways to reduce the nerve messages to the brain (physiology), but the fear and control memories connected to previously experiences are most of what you feel. Control what you expect to experience, and pain is reduced.
Some of what I initially learned about coping with pain came from a good physician friend in Dallas. I didn’t know she had sickle cell disease until she vanished for a few weeks without notice, and when she came back I asked about her ‘vacation’. She’d been in the ICU with acute chest, refusing intubation because she was terrified of leaving her children motherless. She had natural childbirth, because “after sickle cell pain, labor was nothing”. I learned about not being believed, feeling helpless, and resolved to do research so patients with SSD would be believed. I also worked to tell people living with chronic pain the secret codes to be taken seriously, heard and seen when pain flares enough for the emergency department.
When I was lecturing about needle pain in Wisconsin, I met a young woman named Regina who taught me the MOST of anyone ever. Despite hundreds of surgeries and often being wheelchair bound by her juvenile arthritis, she was a leader in the child life specialty field…and one of the most hopeful people I have ever met. She said, “Very little fixes the problem that causes pain. Surgery, prescription anti-inflammatories, maybe, but not much makes it go away. Physical options are SO much more plentiful – heat, cold, pressure. The most important is doing things to keep your mind from noticing, and having the option to try something new or a new combination so you don’t lose hope. What makes pain better is always have an option.” She was the one who suggested the inverted pyramid model of options.
So, after about 11 fractures at about 6 different times in my life, including a neck injury that caused me to be intubated for 5 days and a rotator cuff tear that the orthopedist said “will need surgery because I’ve never seen a bicep tendon rip that angry”, here’s what I’ve learned and done.
Before the TED and the rotator cuff, it wasn’t uncommon for me to get intense neck spasms, and once I video blogged about all the different things I used to avoid opioids. I believe I can stave spasms off better now that I know some brain-body tricks. I will say that the What Works for Pain workbook has a lot that I do when I notice pain early – magnesium, hydration, stretching, sleep hygiene (like not eating or drinking 4 hours before bed). Here’s how I worked my way out of the MORE intense rotator cuff pain that for 6 months I was sure would keep me from every doing what I loved fully again, and that is similar to what I hear worked for people with chronic pain from many causes.

- Learn from a PT the muscles that were weak and needed strengthening. Most pain after an injury comes from the little support muscles that grow and outstrip their blood supply. The lack of oxygen when they get beefy taking the load they’re not designed for is what hurts. Then I’d DO the exercises and stretching, at least once a day.
- Use vibration and HEAT for about 30 – 40 minutes, to increase blood flow to the muscles that were overused, and when I’d feel an early spasm.
- Use vibration and COLD on the areas that were inflamed, to get more blood flow there but stop the inflammation cascade, for about 20 minutes. When awoken at night I’d use the thin ice packs and switch them out two or three times for new frozen ones until I could go back to sleep.
- Find out from the PT how far I could stretch without damaging myself further. Once I knew what was safe but painful, I’d reach the point of pain, take a deep breath, and tell my brain this amount of pain was helpful, I was safe, stop bothering me. I’d use the “count the number of holes in a sentence” trick and focus on another area of my body to push further into the stretch.
- Any time I feel the sharp sour pain that would wake me when the chronic pain was at its worse, I’d focus on diaphragm breathing, or another area of my body that didn’t hurt, and position my arm to be supported by lots of pillows and again say “this isn’t dangerous, don’t worry about this kind of pain” to my brain.
- Work out at least 10 minutes a day with elevated heartrate. There is a protein in the brain called Brain Derived Neurotrophic Factor, that improves both thinking and the plasticity to change pain pathways. The strongest way to increase BDNF is exercise, starting at 10 minutes and elevating your heart rate by 20%. If I feel my shoulder beginning to hurt again, it’s usually because I haven’t done 10 minutes of elliptical or burpees or something else obnoxious.
- Concentrate on what I like doing. Once I got the go ahead from PT, I started swimming again. Yeah, it hurt, but I kept telling myself that swimming is what I like to do, it’s what I want to do until I’m 80, so just do it then and shoulder, quit whining.
Dr. Kevin Vowles and Lance McCracken do research on Acceptance and Commitment therapy. You accept that there IS pain in this particular moment, and focus on committing to the events that make life worthwhile.– Or to quote Nietzsche “he who has a why to live can bear almost any how.” The courage is ignoring pain, and practically committing to activities that in sum WHY to live. Go fishing. Go to your daughter’s wedding. This has now been well researched in adults and children, and was twice as effective long-term compared medication. Viewing pain as an annoying new normal, rather than an identity shift, was actually more effective at reducing pain and depression.
Finally, I have an advantage that of course most people don’t have: since I work with pain for a living, I have people who constantly tell me how they overcame pain. Some say they didn’t realize how chronic pain was a companion, and there is some loss when it’s gone. Some say they learned meditation, or microdosed, or cut off circulation to an area to make it hurt WORSE, then it got better because they had control. Whatever the technique or reason, I know so many people who overcame pain or work daily to make it manageable, I believed it could be done. And now that I’ve come to fully accept my “more comfortable” over a process of 7 months, I’m not afraid of pain any more.
NOTE: If you’re on opioids and want to wean, there are FDA approved electrical stimulators that can help partially activate the opioid receptors to reduce cravings. Buprenorphine is also a partial agonist, but won’t allow for a gradual reduction of pain relief, just help sate the cravings and withdrawal symptoms. Most weaning programs reduce opioids by a certain percentage over time periods.