Blog
Attacking the Opioid Crisis on a Budget: 8 Innovative Ideas
Political talk is cheap, substance abuse programs are expensive, and the nature of the crisis demands fast action. Sadly, while an official ‘public health emergency’ declaration helps, it doesn’t give a quick infusion of cash to help embattled front line substance abuse workers. To allocate funds, the Health and Human Services (HHS) budget (that currently cuts $4B in funding) must be revised so that Congress has funds to allocate. As it looks like the crisis will continue to be fought on a shoestring, in addition to immediate definitional changes to access existing funds, it’s time to get the biggest bang for addiction intervention bucks: prevention innovation.
Addiction is heartbreakingly difficult to combat, with high failure rates and costs to society. The substance abuse programs that need money are obvious: the acting HHS secretary can allow Medicaid to reimburse opioid abuse treatment at mental health centers, negotiate reduced costs for naloxone, and mandate Medicaid reimbursement of proven addiction medications. (This actually saves systems money – mean health care costs with addiction medication treatment = $13,578; vs. with no addiction treatment = $31,055) . Waiving the requirement for naloxone prescriptions will save lives. But since resources are scarce, focus on increasing community health access for addicted pregnant mothers. Addressing addiction before birth saves $55,000 in treatment costs for neonatal dependence, with lifelong savings in education and law enforcement costs.
Since the era of “Oxycontin doesn’t cause addiction”, between 40 and 80% of opioid abuse has been attributed to initial medical use for pain. These studies underestimate the medicine cabinet availability for experimental teens – they weren’t in pain, but someone was. As part of an opioid legislative package in Georgia, pharmacist Rep. Buddy Carter sought help from pharmaceutical companies, noting “Once you get past Tramadol and a couple of others, there is nothing else for us to use [for pain], there is nothing else for us to prescribe.” This perspective is exactly why we have an opioid problem – we’re focusing on drugs, not the problem of pain that got us there. Want fewer addictions? Put fewer pills in circulation.Here are some obvious and some less-intuitive ideas:
- Lower the quantity of pain medications per prescription
Pain is personal, but there is some generalizability of duration of pain for normal recovery. Tier pain management clinical scenarios, and limit scrips for 24, 72 hour, and (rarely) 7 day home recovery.
- Redefine chronic pain
“Chronic” has been defined as pain lasting 3-6 months. Opioids are poor choices for most patients with chronic pain, but by three months of treatment, addiction already exists. We need a new treatment category for pain lasting over 7 days, and must change our focus from treating chronic pain to promoting movement and function.
- Cover initial visits for pain to physical therapists
Pain is usually physical – physical problems require physical solutions. We need to cover visits to physical therapists prior to physician authorization, paying for longer treatments to rehabilitate misused muscles, strengthen, and change movement habits. PTs won’t prescribe Percocet.
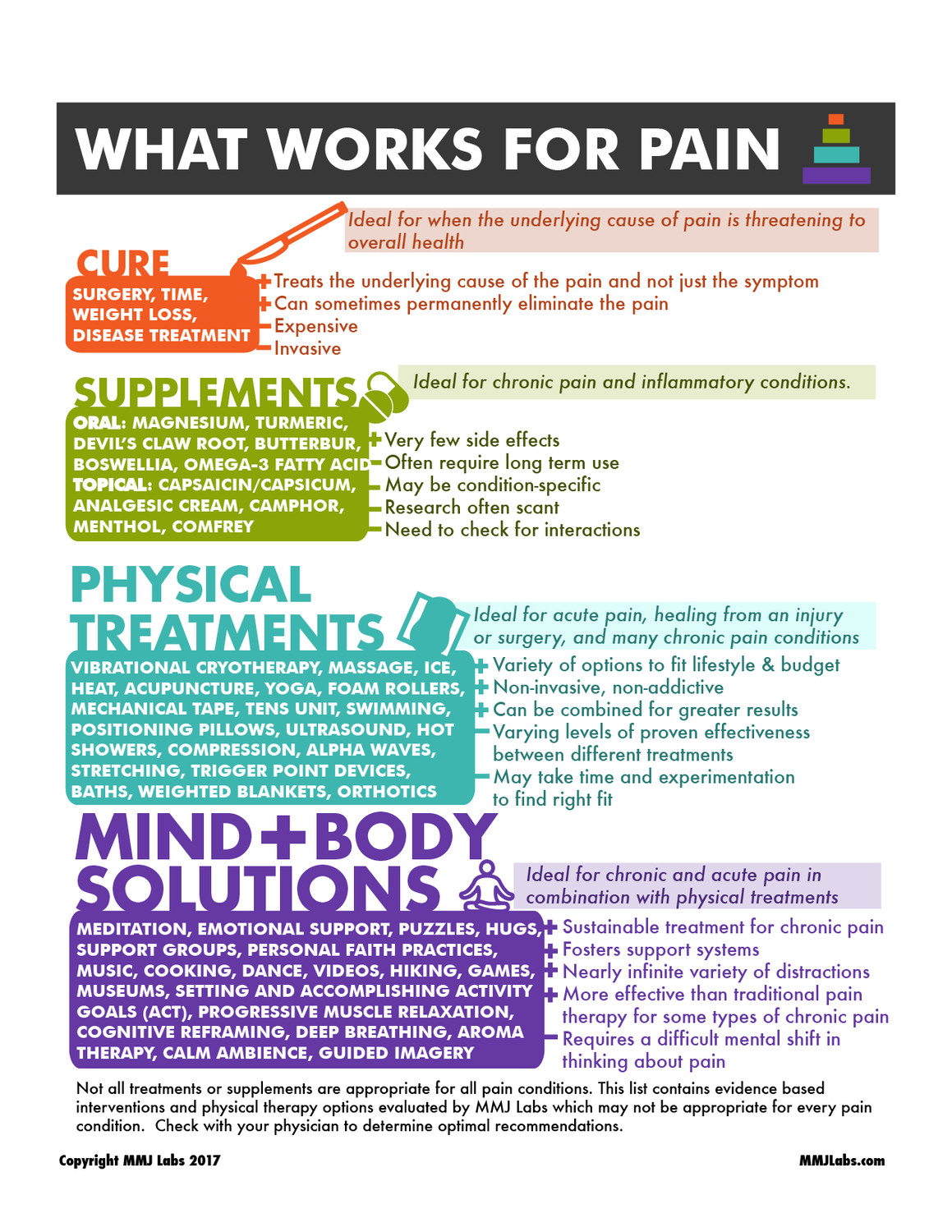
- Require non-pharmacologic recommendations with every prescription
Prescribing medications is a physician’s super power – we study long and hard for the ability to help people in pain with a prescription. To change addiction, we have to change physician behavior
will transform you. For many years androsterone was considered the primary male hormone until testosterone was discovered from concentrated testicular extracts many years later Steroids for sale online The glutamic acid-sports pharmacology interconversion is of central importance to the regulation of the levels of toxic ammonia in the body,
by teaching alternate evidence-based options for pain. This will take a while, so for now, teach pain patients they have options. When patients have a list of non-drug interventions (like the free download of the list below) the ability to choose gives control, reduces fear, and helps diminish the incorrect perception that drugs are first line pain relievers.
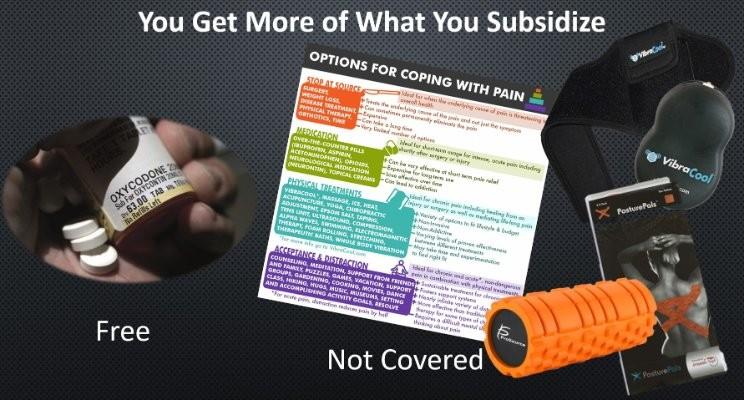
- Cover pain relief devices and office education
The Centers for Medicaid and Medicare pays for pills, but won’t pay for low cost home devices, even when used to reduce opioid intake. BakBalls, VibraCool, NeckRest, Posture Pals, soft tissue rollers, all are over the counter and used by clinicians for patients’ pain. To avoid covering a device that a patient finds too cold, or an electrostim unit when a patient hates the feel of electricity, reimburse therapists for office trials.
- Create non-pill pain management lists post surgery
Doctors don’t have time to cover exhaustive options, but there are evidence-based nonpharmacologic treatments NOW to address chronic and post-surgical pain. University of Michigan offers a “Poke Plan” for needle pain, University of Iowa has a laminated list from creams to Buzzy – offering treatment option menus to patients is not just good service, it’s good science. Menu-selected treatments benefit from belief bias, choice-supportive bias, confirmation bias, selective perception, and even the “IKEA effect”– you like a pain plan more if you made it yourself.
- Give injury, chronic pain and post-surgical patients a $200 budget for pain services and products
Pain relief options aren’t useful if they’re unaffordable while opioids are free. If a patient hates stretching but loves massage, don’t waste time and money prescribing a yoga class. Massage, thermal treatments, yoga classes and chiropractor visits topped Consumer reports lists of effective pain management treatments. Pay for them.
- Use available pharmacogenomics testing to predict de novo abuse
Opioids in particular have variable metabolism. Caucasians with variations of the CYP2D6 enzyme metabolize opioids poorly – they may get poor relief from opioids, but more importantly are less likely to become addicted. In contrast, ultra-rapid metabolizers have greater risk of overdosing, and likely addiction. The genetic test is currently available, and the cost and clinical benefits are being tested by Indiana University. Funding to make a rapid bedside test available could help both pain treatment and prevent susceptible patients from getting opioids at all.
- Don’t even think of putting more money toward the drug war. Aggressive law enforcement keeps illicit drug users and pregnant mothers from treatment, and has not been proven to reduce use. A 2012 article in The Lancet argues international drug conventions may have increased availability. No additional funds here.
Treating addiction is astronomically expensive. Drastically curtailing opioids in circulation can save money as well as lives at a fraction of the cost. Declare a national emergency, yes, and PLEASE pay for addiction medications, but let’s use this ‘public health emergency’ opportunity to change how we think about and pay for pain.