Blog
Pain and the Pendulum – 5 ways the opioid panic could evolve pain management
“The greatest evil is physical pain.” – St. Augustine
Physical pain is intertwined with safety, the base of Maslow’s hierarchy of human needs: pain trumps other problems. In the 1990’s, the US medical system began focusing on the problem of undertreated pain, thus beginning the pendulum swing toward pain measurement and management. The epidemic of opioid deaths reveals an apex of complications that result from any pendulum swing, with blame directed at pharma, regulatory guidelines, and physicians’ prescribing practices. Without understanding the forces involved, we risk curtailing the availability of relief to those whose suffering started the swing. Without consideration of consequences, we could lose the opportunity to truly relieve suffering revealed by the inadequacy of our pharma-focused solutions. Solving the problem of pain requires shifts in the understanding of pain, the language of relief, and the regulatory landscape and lack of other options that promote prescriptions.
Recent articles blame the over-measurement of pain for the rise in addiction to painkillers. In reality, opioid prescription was already surging before the Joint Commission began including pain management as a quality marker in 1991.
What promoted a hospital pain focus was research showing a clear discrepancy in acute pain management by age, race, and gender. The greater understanding that pain impairs healing and that inadequate relief increases the risk of chronic pain was underscored by an empathy gap of uniform pain management by physicians, fueling the focus on pain before “satisfaction” was even a thing.
Aggressive and often scientifically inaccurate marketing of opioids greatly benefitted from this push to better serve patients’ pain. A fantastic article by Dr. Art Van Zee chronicles the unprecedented rise of OxyContin since 1996, wherein Perdue Pharma conflated chronic pain “management” with opioid prescription.1 The company paid $634 million in fines for representing addiction risk as less than 1% rather than the 20-30% typically reported in chronic pain users.2 Opioids have two millennia of history for effective acute and cancer pain management. A growing body of data, however, disconnects efficacy of treatment for acute from chronic from cancer-related pain management. Different treatments are successful for different pain situations, and one pill does not fit all.
As the CDC proposes to curtail opioid use, there is an urgent need to educate physicians about other pain options in order to preserve the gains in appreciation of pain’s importance. For example, while three studies show that ibuprofen is superior to codeine for home fracture pain management, Lortab is still prescribed. Is this habit, lack of knowledge, or a deeper problem with the way we approach health? NPR reports on the growing body of evidence supports mindfulness, massage, stretching and vibration for pain. These modalities are still underused, however, in large part because physicians aren’t trained on them, and the pain management specialists aren’t consulted (or reimbursed) until chronic pain has become established.
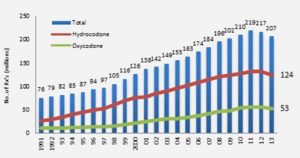
Here are five solutions that need to be part of the national dialogue on pain, before baby, bathwater and tub all go out the window in an attempt to stop addiction. [Note in the graph above that prescribing trends are actually already declining. Legislation follows media frenzies, but media frenzies follow data a few years behind.]
First, separate acute from chronic pain while training physicians and the public about how the transition occurs. The CDC opioid guidelines, actually, explicitly note that they’re discussing non-cancer, non-acute pain. When it comes to opioids, manage acute pain aggressively, chronic pain cautiously. Rating pain is necessary in the acute setting, as once pain becomes unmanageable, fear, cortisol, catecholamine production, and other physiologic pathways cascade. Pain is personal, and without meticulous rating based against a patients’ own perception the right titration of medication to stop the pain cascade won’t be achieved. Rating chronic pain, however, is counterproductive, pulling a focus toward the problem. Multiple studies demonstrate that accepting some degree of pain and committing to doing valued activities despite the pain is more effective in the long run than treating the pain itself.3
Second, combat patient impatience by redefining the goal of pain management. When an internist on NPR said that pain is part of healing, the message might better be that healing results in reduction of pain. Pain relief is a process, not a prescription. Don’t promise pain-free. Prescriptions are given like magic bullets, biasing patients to expect more than they will get. This era of iPhone-instant gratification has to stop when it comes to our bodies. Slow food and slow medicine are gaining ground; slow pain improvement through multiple modalities must become a mindset with chronic pain.
Third, subsidize aggressive education of physicians AND THE PUBLIC on non-pharmacologic pain solutions. $50B is spent out of pocket by patients on pain each year, with total pain health expenditures at $300B.4 The vast preponderance of the $300B is on prescriptions, with $34B for alternate therapies, and only 2% spent on medical devices. This is utterly disproportionate to what patients say works – in a 2011 Consumer Reports survey of 45,000 patients, drugs usually finished second or third. We’re paying 90% of our healthcare costs for the 2nd or third most effective treatments. Medical devices, like massage and ice, aren’t reimbursed so manufacturers don’t have a market push to make them more available, even when proven effective. The centers for Medicaid and Medicare withdrew support for TENS units because they were not shown to have chronic pain benefits, but didn’t replace this with other proven modalities. Massage, vibration, and vibration/ice combinations all have strong data, but without a reimbursement plan, they are bundled losses for hospitals or out of pocket costs for the hurting.
To address pain, the primary solution is to eliminate the physical problem or disease state. Second tier solutions are usually pharmacologic, with NSAIDS (ibuprofen) and other non-addictive medications at the core. Options for both first and second tier are finite; options for non-pharmacologic and alternate are truly almost limitless. Educating toward this mindset before chronic pain develops could be funded by the fines pharma companies are paying, or through imposition of a surcharge on companies who have raised their prices on opioids more than the cost of inflation in the past 5 years. There’s little profit margin in promoting non-pharmacologic solutions, so external funding is needed to compete with superbowl pharma ads.
Fourth, reorient reimbursement. You get what you subsidize – use of opioids for pain is facilitated by reimbursement. Currently, the equation is patient + problem = prescription. In reality, most solutions would be prescription OR lifestyle change OR [variety of non-drug solutions]. When a scrip is included, human nature favors the least complicated…and the cheapest. This is a pure CMS problem, essentially subsidizing pain drug manufacturers. We must remove pressures favoring prescription pain solutions, by taking away the cost benefit of drugs for patients. If a patient has to pay out of pocket for a $60 VibraCool massaging ice device that I make, or gets 125 OxyContin for free, what do they choose? There are a number of ways to implement this solution: reimburse reusable pain devices with FDA 510K clearance; match acceptable funds for prescriptions with alternate therapies that work; identify patients at greater risk of chronic pain and pay for chronic pain evals before chronic pain develops. Reimburse pain patients for EITHER ½ the cost of a massage or a prescription. The difficult systemic solution is to make it easier for a physician to prescribe a non-opioid therapy than a pharmacologic one.
Finally, change the language of empathy from drugs to options. When a child comes into our emergency department with a broken arm, almost everyone prescribes hydrocodone. For an emergency physician, giving a scrip says “I care about your pain; I believe you hurt”. This language of caring is inaccurate given the research, but just telling a patient that ibuprofen is better feels less compassionate than giving a scrip. Doctors don’t have good materials to give for other methods of coping. Patients have been taught that “serious problem = scrip, and if they don’t get one they’re being shortchanged. We need to make materials that give options for pain to substitute for the scrip.
At the heart of this controversy is the desire to relieve the greatest of evils, physical pain, without replacing it with the evil of addiction. Fortunately, the solutions of education and alternate therapies present an opportunity that could cut the cost of pain management in half. The great danger in this debate is the risk of pain relief being crushed between two noble goals. Measuring pain to facilitate effective and equitable treatment of suffering is an enormous gain made in the past two decades – as opioid prescription is already falling, let’s use this awareness as an opportunity, not a pendulum swing into the painful past.
- Zee AV The promotion and marketing of OxyContin: Commercial Triumph, Public Health Tragedy. Am J Public Health. 2009 February; 99(2): 221–227.
- Hojsted J, Sjogren P.Addiction to opioids in chronic pain patients: a literature review.Eur J Pain2007;11:490–518 [PubMed]
- Vowles KE et al. Acceptance and commitment therapy for chronic pain: evidence of mediation and clinically significant change following an abbreviated interdisciplinary program of rehabilitation. J Pain 2014 Jan;15(1):101-13
- Gaskin DJ, Richard P. Relieving Pain in America: A Blueprint for Transforming Prevention, Care, Education, and Research. http://www.ncbi.nlm.nih.gov/books/NBK92521/